From The New York Times, I’m Annie Correal, in for Michael Barbaro. This is The Daily.
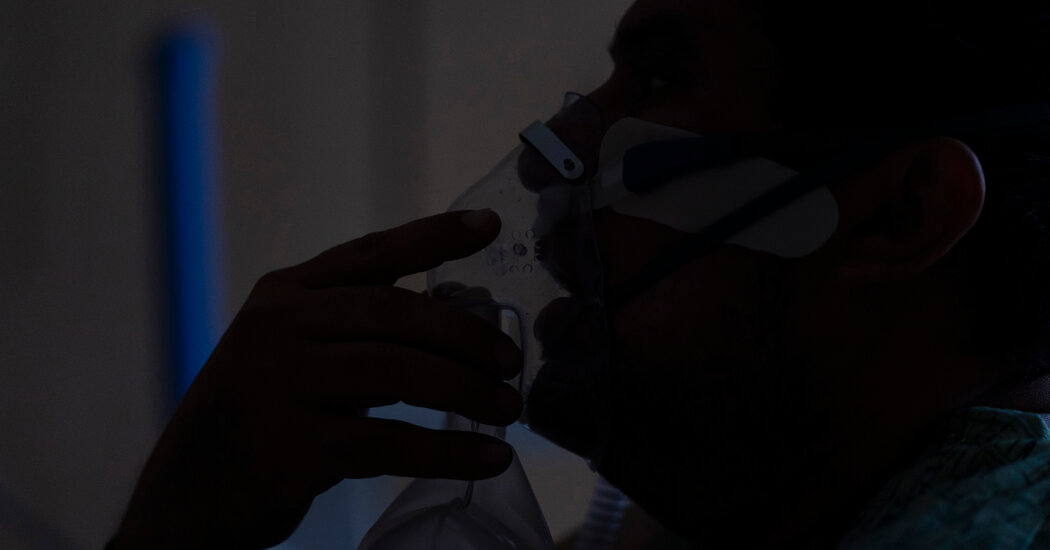
Today: Despite its reputation for mild illness, the Omicron variant is fueling a staggering rise in hospitalizations around the country. I spoke with my colleague, Emily Anthes, about why doctors and nurses inside those hospitals say that this phase of the pandemic feels so different. It’s Tuesday, January 11.
So Emily, you’ve been reporting on hospitals across the U.S. and the challenge that they’re facing at this particular moment in the pandemic. Can you tell us about what you’ve been hearing?
Absolutely. So cases have been skyrocketing in recent weeks. If you look at graphs of cases, they’re basically vertical, and the highest case numbers we’ve seen at any point in the pandemic. And hospitalizations, which tend to lag behind cases, have started to rise, too.
And in some of the early Omicron hotspots — New York, New Jersey, Massachusetts, elsewhere — hospitals are being flooded with new patients. They’re just being inundated. Emergency rooms are filling up. There aren’t enough staff to care for all these patients. And that might seem like a bit of a paradox because we, ourselves, have covered a bit about how evidence is emerging that this variant, Omicron, might be a bit milder than Delta, which caused some of the previous surges.
So we wanted to try to figure out what was at the heart of this tension. If this variant was causing milder illness and so many Americans are vaccinated now, why are hospitals filling up?
- speaker
-
This is [INAUDIBLE]
- emily anthes
-
Hi, this is Emily Anthes, calling from The New York Times. How are you?
- speaker
-
Good, good. Can you hear me OK?
- emily anthes
-
I can.
So several of my colleagues and I —
- azeen ghorayshi
-
— are trying our best to talk to as many hospitals —
— including my colleague, Azeen Ghorayshi —
- azeen ghorayshi
-
— to sort of find out what’s happening on the ground —
— started calling doctors and hospitals —
- speaker
-
Hold on. Let me get Dr. Mays on the line.
- emily anthes
-
— all over the country.
- speaker
-
Here in Miami-Dade, our vaccination rate is high.
Florida —
- speaker
-
We are the main university hospital in Winston-Salem, North Carolina.
— North Carolina.
- speaker
-
— the state of Georgia and others.
— California, Maryland, Texas, Rhode Island.
- speaker
-
Yes, I am hanging in there.
And we asked them —
- azeen ghorayshi
-
Can you just describe a little bit more just how this does feel different? I mean —
What are you seeing and how is this surge different?
- speaker 1
-
Our hospitalizations are nowhere near what they were at the height of the epidemic. But they are higher than they were in the summer when we had a bump up with Delta.
- speaker 2
-
Very early in the pandemic, the thing that health systems everywhere were worried about were running out of ventilators. And now the real limitations are obviously physical bed space.
- speaker 3
-
I mean, it’s now to the point where it’s just kind of crazy. It’s crazy.
So what did doctors say about why the hospital system is under such strain at this moment?
Well, there are two big reasons. And the first is just that Omicron moves really, really fast. Several weeks ago, I talked to some forecasters and some modelers who were trying to predict how this would all unfold here. And at the time, they were saying this surge would probably peak in mid to late January with something like 400,000 new cases per day in the U.S.
Well, here we are in early January, and we are already at nearly 700,000 cases a day. We just blew past that forecast. And this thing has moved so much faster than even the experts predicted.
So even if Omicron is half as severe, if it’s causing twice as many infections, you’re sending the same number of people to the hospital.
- speaker 1
-
The last two weeks have really, really picked up.
- speaker 2
-
It’s very hard. It’s very concerning. We have more patients in the hospital than we’ve ever had before with Covid.
So hospitals just aren’t used to the volume.
- speaker
-
We’re overwhelmed. We’re overwhelmed with Covid and other diseases, right? I mean, in the first Covid wave, all of the patients stopped coming to the hospital. Right now, we’re seeing everybody else plus the Covid patients.
- azeen ghorayshi
-
Right.
- speaker
-
You know, we were at a low point. And then all of a sudden, in comes the Omicron 800-pound spreading gorilla to Houston. And lo and behold, we’re off with a case-doubling time of roughly, once again, rounding to two days — very, very traumatic.
And what doctors are telling us is that this variant is so infectious that they’re finding it in a lot of patients that aren’t even coming in for Covid.
- speaker
-
People who are admitted for something else who incidentally have Covid, that’s a change.
- emily anthes
-
Yeah.
They’re coming in to give birth. They’re coming in because they broke a bone. They’re coming in because they had scheduled a hip replacement a month ago. And when they get tested for the virus, they’re turning out to be positive.
- speaker
-
About a third to a half of the people coming in these days have Covid.
- emily anthes
-
Mm-hmm.
- speaker
-
It’s an amazing number, right?
- emily anthes
-
Uh-huh.
So these incidental infections are part of what hospitals are seeing now. There isn’t really good data on this, especially nationally. But there’s a significant share of patients in hospitals right now who have these incidental infections. So estimates we got ranged from 20 percent to 65 percent at one New York hospital.
So you’re saying that at this hospital in New York, two-thirds of patients coming in for anything — for a hip replacement, or because they’ve given birth, or broken a bone — are turning out to test positive for Covid?
Yeah, and we wouldn’t have even found a lot of these cases, if not for the fact that a lot of hospitals have started testing all of their patients for the virus. So this thing is everywhere.
Right. But just to make sure I understand, these people who come in for other things, they would have come to the hospital regardless. So how is that an added strain on hospitals?
Well, it is true that a lot of them probably would have been coming into the hospital anyway. And the good news is that a lot of people with these incidental infections may not get very sick from Covid. But they can still pose an added strain on hospitals.
- speaker
-
Even though they’re not sick with Covid, they still have Covid and they’re still infectious. So you still need to put them in isolation. You still need to treat them as patients who have potentially transmitted Covid in the hospital, right?
- azeen ghorayshi
-
Right. Which takes more space and more staff.
- speaker
-
Correct, correct.
And part of that is because they need to be isolated while they’re in the hospital to prevent them from passing the virus onto others. And that requires resources and staffing. And, in some cases, having one of these incidental infections can worsen their own outcomes that can interact with whatever reason it is there in the hospital. And these patients may fare more poorly than they otherwise would have.
OK so more patients are coming in with Covid than ever before. And that’s overwhelming hospital systems. What’s the second reason that hospitals are facing a bigger burden today than during previous surges?
- speaker
-
Well, you have to understand that the major concern right now is staff.
This was a very clear answer from every doctor we talked to.
- speaker
-
Staffing limitations.
A huge concern —
- speaker
-
There’s a shortage of staff.
— staffing.
- speaker
-
Frankly, today I’m more worried about staffing than I am being overwhelmed by patients.
Many hospitals were already really struggling with staffing shortages, even before this surge. Over the course of the last two years and the pandemic, a lot of health care professionals and hospital staff have left their positions.
- speaker
-
If we were to compare it to a year ago when we thought this was the worst, the difference now is our staff are tired. Our staff are getting sick and calling off work. And we entered it with fewer staff than we ever had before.
Due to stress, burnout.
- speaker
-
Choosing to either pursue other careers or different pathways.
So even before this surge started, hospitals were really strapped for staff.
- speaker
-
So we’re entering with higher numbers than we saw a year ago, with fewer people to care for those patients. We can take up to about 140 patients normally. Right now, we’ve reduced that, though, because we don’t have enough staff to care for patients.
And then you layer on top of that the fact that we’re dealing with this highly contagious variant, and lots of hospital personnel are catching it. And that is further depleting the ranks of hospital staff.
You know, it’s not just doctors and nurses.
- speaker
-
We have a reduced number of certified nursing assistants.
But they’re also short on behavioral therapists —
- speaker
-
— radiology techs —
— and pharmacists.
- speaker
-
— cafeteria staff —
— and custodial staff. Everyone that it takes to sort of make a hospital run smoothly and run well, the entire operation is struggling under the weight of this surge.
I heard that they had, in some places, called in the National Guard to assist, to help people because of that shortage in staff?
That’s right. And some of the doctors I talked to said that was actually really welcome and exactly what they needed, were more hands right now. Obviously, that’s not a long term solution for staff shortages. But right now, it’s really all-hands-on-deck. And they are happy to have whoever they can get.
So to recap, what we’re looking at is an enormous surge in cases driven by this highly infectious and fast-moving variant, combined with extreme staffing issues. We’ve got all this attrition, people quitting after two years of the pandemic, and doctors and nurses and janitors out sick.
So what is the impact of that on patients?
The impact is enormous.
- speaker
-
I can’t speak for each and every Maryland hospital, but several of our hospitals in Maryland have declared they need to go on crisis standards of care.
A lot of the doctors we talked to said that they had already stopped doing or were considering stopping doing any sort of non-emergency procedure — all these elective surgeries.
- speaker
-
So our hospitals, we’ve curtailed surgeries. And the important surgeries — like we think of them as elective. But if you have breast cancer and you need an operation, I don’t think anybody really thinks that’s elective.
Really, they can be for quite serious conditions. These might include things like cancer surgeries, transplants, heart surgeries. And they’re being canceled or postponed because hospitals just don’t have the staff and the bandwidth right now.
- speaker
-
You know, here’s a scenario. Here’s a perfect example. You have an aneurysm. It’s not going to hurt you right now. It doesn’t look like it’s getting bigger. But we should probably operate.
So now I come home from that doctor’s appointment and I tell my family, my God, I got this thing in my head. If it bursts, right, that’s like having a stroke, that’s awful. Like, this could be a big deal. And then their doctor calls them and says, you know what? We’re going to wait another week or two. Like, there’s not a single scenario I can run through my head where a human being can feel calm and collected about that.
Another doctor we talked to said that some of these surgeries are essentially canceling themselves because people are coming in for surgeries they’ve scheduled and testing positive for the virus, which means that the surgeries then have to be postponed and care is delayed.
So when hospitals get overwhelmed and staff get stretched really thin —
- speaker
-
There’s shortages of ambulances.
— everybody’s care suffers.
- speaker
-
— people with heart attacks might not get to the hospital as much. The E.D.s are absolutely full and crushed with patients, a huge set of safety issues.
We’ll be right back.
So Emily, you’ve explained how hospitals can be under such stress at this moment, even though Omicron seems to be presenting as a milder version of the virus. Do you have a sense from your reporting how long this will last? Is there a world in which this is just a short-term hit on the health care system?
Well, in South Africa it took about three to four weeks for cases to peak. And then they started declining. It’s not clear yet if the same pattern will hold here in the U.S. But even if it does, we know that hospitalizations tend to lag about two weeks behind cases. And deaths tend to lag about three weeks behind cases.
And here in the U.S. right now, our cases are still rising. It doesn’t look like we’ve hit that peak yet. So most doctors we talked to unfortunately think that it’s going to get worse before it gets better.
Hmm.
And even if the immediate crisis is short-term, it could have lasting consequences. Delaying these elective or non-emergency procedures could cause them to pile up, could cause patients to worsen. So when they do eventually get medical care, they are sicker and have worse outcomes. And they could further worsen the staff shortages that already exist by driving more people out of the health care field.
The other reason to be concerned here in the U.S. is that we still have a lot of people in this country who are unvaccinated. And Omicron is not necessarily mild for them.
So then are places where more people are vaccinated more likely to fare better with this most recent surge?
So it’s a little bit hard to draw any conclusions about that right now. And part of that is because of the patterns of when and where Omicron arrived first. As it happens, some of the areas of the country that got hit first, and hardest, and fastest with Omicron are areas that have pretty high vaccination rates.
They are places like New York City, New Jersey, Massachusetts, which are highly vaccinated areas. So these are the places that are really seeing hospitalizations surge right now, while some of the less vaccinated places in the country are a little bit behind. So we have to wait for more time and more data to make those kinds of community-level comparisons.
But what we do know is that the overwhelming majority of patients who are getting severely ill and ending up in I.C.U.s are the unvaccinated. Omicron can be quite serious for these patients. And doctors told us over and over again that these are the patients who are on ventilators, these are the patients they worry about, these are the patients who are dying.
- dr. ryan maves
-
Hey, how are you doing?
- emily anthes
-
Good, how are you?
- dr. ryan maves
-
Gainfully employed.
- emily anthes
-
Yeah, well thank you so much for making time —
So I talked to a critical care doctor in North Carolina, Dr. Ryan Maves. And he’s a former Navy captain who was deployed to Afghanistan.
- dr. ryan maves
-
And I’ve just — over these last two years, I’ve never seen deaths like this before. Right? You know, and I’ve been to war. And this last week was a particularly poignant reminder of that.
And he said that what he saw recently in the hospital and especially in the I.C.U. was among the worst weeks of his career. And it actually reminded him of being back at war.
- dr. ryan maves
-
And I’ll say, every vaccinated patient whom I’ve cared for in the I.C.U., they are people with kidney transplants. They are people with leukemia, lymphoma, people with cancer, people for whom immunization is protective, but they’re less likely to benefit from it, right? But yeah, it’s overwhelmingly unvaccinated people. And it is skewing younger than it used to.
Mm-hmm.
- dr. ryan maves
-
You know, many more people in their 40s and 50s and many of them dying. And it’s a grim feeling, watching people who are your own age and maybe not that much older than you dying of an entirely preventable illness.
And I think there’s a lot of frustration that America’s not more vaccinated at this point, which could have fended off the worst of this surge.
- dr. ryan maves
-
It’s a few things. It’s all at the same time. It’s sad. It’s infuriating. And it is, a lot of times, very difficult to be empathetic.
There’s a doctor in the suburbs of Chicago, Dr. Bob Manam, who said this really explicitly.
- dr. bob maman
-
So this is something that we’re constantly getting emails from the hospital saying, you’ve got to keep your empathy up. You have to — and when you read the chart before you go into the room, you’re, like, just shaking your head. But then when you go in there and you talk to the individual, you do definitely feel very sorry. But it didn’t — it’s like it is a 100-car wreck on the road. And this is the 101st car. Everybody’s been saying slow down, the streets are icy, be careful. Wouldn’t you want to take some sort of precaution?
So where does that leave doctors and hospitals in this moment?
It leaves them in trouble. I think a lot of us think that we’ll probably pull through this Omicron wave just fine. And most of us, especially those of us who are vaccinated and boosted, probably will. But I don’t think we can forget the toll that this is taking on health care workers who have already been pushed to the limit and who are now being pushed even further by this surge.
- speaker
-
To me, that’s the main story, how bad and how big this really is.
You know, my colleague Azeen talked to a doctor in Maryland, Dr. Gabe Kelen, who said he’s not even sure that Americans really know how crushed hospitals are right now. But just because they don’t know doesn’t mean it’s not happening.
- dr. gabe kelen
-
The last time, in the first really big crush, I think we reached a peak of about 1,500 hospital beds for Covid patients. This morning, we’re at 2,700. I mean, with an acceleration of 200-300 a day. You know, it’s like going down Great Six Rapids. You just can’t ever quite catch your breath.
And the public just doesn’t know. And maybe they’re just too tired at this point as well, to care.
Thank you, Emily, very much.
Thanks for having me.
The number of Americans hospitalized with Covid-19 has now surpassed last winter’s peak, according to the U.S. Department of Health. As of Sunday, 142,388 people had been hospitalized, surpassing the previous record set in January of last year.
We’ll be right back.
Here’s what else you need to know today. The Biden administration said on Monday that private insurers will soon be required to cover the cost of eight at-home coronavirus tests a month. The requirement is designed to address the high cost of at-home tests, which has discouraged many Americans from using them. Under the plan, people will be able to buy the tests at no cost from pharmacies approved by their insurance, or buy them elsewhere and file for reimbursement.
Today’s episode was produced by Daniel Guillemette and Asthaa Chaturvedi, with help from Mooj Zadie. It was edited by Mark George and Lisa Chow, features original music by Marion Lozano and Dan Powell, and was engineered by Marian Lozano. Our theme music is by Jim Brunberg and Ben Landsverk of Wonderly.
That’s it for The Daily. I’m Annie Correal. See you tomorrow.